There are changes that happen in your body when you have cystic fibrosis (CF) that you will need to talk to your health-care team about. Many people just think about the lungs when they think of cystic fibrosis (CF), but it can affect other areas of the body as well. Some of the areas of the body that CF affects include:
- the lungs, sinuses and nose
- the liver, pancreas, and intestines
- puberty and fertility
- the muscles and bones
Also, having a chronic condition such as CF can affect your mental health and how you feel about yourself.
Complications
The goal of regular clinic visits is to identify, treat and prevent complications from CF. Understanding the way CF may affect your body will help you share information with your health-care team.
Pulmonary exacerbation
Pulmonary exacerbations are when a person with CF experiences a more severe lung infection. Certain bacteria growing in the lungs can make you sick with more coughing and more mucus and maybe even cause difficulty breathing, chest pain or coughing up blood. You may also have low energy levels and you may even lose weight. Sputum samples and throat swabs help to identify what bacteria may be growing. Antibiotics may be prescribed for pulmonary exacerbations to help fight the bacteria in your lungs. It is also very important to keep up with your airway clearance to clear out the mucus. Bacteria that are often found in the lungs of people with CF include:
- Pseudomonas aeruginosa
- Staphylococcus aureus
- Haemophilus influenzae
If you are having any of the above symptoms, make sure you contact your CF clinic team.
Sinus congestion
The sinuses are air-filled spaces in the head located between the eyes and nose. Their job is to produce and circulate mucus. Tissues in your sinuses can become inflamed and swollen because of a bacterial infection. When this happens, it interferes with drainage of mucus from your sinuses and can cause more mucus to build up leading to sinus congestion. Symptoms of sinus congestion include the loss of smell and taste, headaches, increased need to clear your throat and pain in your face. Sinus congestion can be treated with nasal sprays and nasal saline washes.
Nasal polyps
Nasal polyps are small tissue growths that develop in the nasal passages and sinuses. Nasal polyps likely grow when someone has frequent or long-term nasal congestion or infection. The size of the nasal polyps can vary. If you have large polyps they can cause a blocked or runny nose and even loss of smell or taste. Nasal polyps can be treated with medications and sometimes you may need surgery to remove them.
Liver
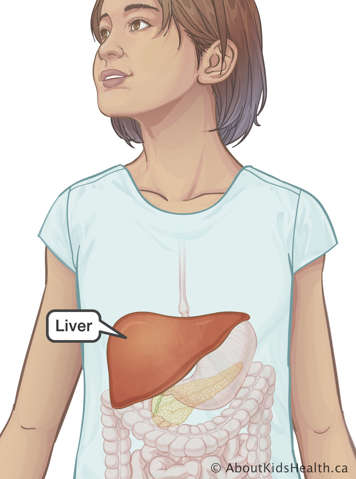
One of the liver’s jobs is to produce bile, a substance that helps break down the fats in our food during digestion. Sometimes the bile that is made by the liver is stickier than normal and can build up in your liver and bile ducts. This build-up of bile can cause irritation, inflammation and blockages, and can lead to scarring or fibrosis of your liver. These changes affect the usual function of the liver.
Regular blood tests and imaging are done to screen for CF liver disease.
Cystic fibrosis-related diabetes (CFRD)
CF-related diabetes (CFRD) is a type of diabetes that only people with CF get. Diabetes is a condition where the pancreas cannot produce enough insulin because of scarring. Insulin controls the amount of sugar in your blood by helping it enter other cells such as the muscles where the sugar is turned into energy. Without enough insulin, sugar cannot be used for energy and your body cannot balance the amount of sugar in your blood. You may:
- lose weight
- feel tired and have low energy
- have low numbers on your pulmonary function tests
- feel unwell
Screening for CFRD starts when you are 10 years old and is usually done every year after that. It is done with an oral glucose tolerance test.
Oral glucose tolerance test
You cannot eat or drink for eight hours before the test. This is often done by not eating or drinking after dinner and having your test first thing the next morning. When you arrive for the test a blood sample will be taken to measure your blood sugar levels. You will then drink a special orange-flavoured drink. Two hours later another blood sample will be taken. This test measures the amount of sugar (glucose) in the blood at that moment. The blood sample can also be used to look at something called hemoglobin A1c (HbA1c). Your HbA1c measures your average blood sugar levels over the past 3 months.
It is also important to monitor blood sugar levels if you are taking oral prednisone as this medication can increase blood sugar levels.
If you have CFRD you will continue to be followed by the CF clinic with help from an endocrinologist and diabetes care specialist. You will be given education and recommendations on how to manage CFRD such as healthy eating, monitoring blood sugar levels and adjusting insulin doses.
Distal intestinal obstructive syndrome (DIOS)
Distal intestinal obstructive syndrome can happen when mucus builds up in the small intestine. This slows down the emptying of your intestines which causes stool to get backed up. You may have stomach cramps, vomiting, diarrhea and pass fewer stools. You may need an abdominal X-ray to see if you have DIOS. If you have DIOS it can usually be treated by drinking more fluids and taking laxatives.
To help prevent DIOS it is important to eat regularly, take your enzymes as prescribed by your health-care team and drink fluids to help with the digestion of food.
Puberty
People with CF usually go through puberty on average 18 months later than their peers. Females with CF may be between 15 and 17 years old before they start to go through puberty and males can be older than that. Having a lower body weight affects when you start to go through puberty so make sure you are getting enough calories and nutrition.
Fertility
Females with CF still produce healthy eggs and many can get pregnant without any sort of treatment. Fertility problems in females can be related to their overall health. For example, if they are frequently ill due to infections or are underweight because of problems with breaking down food, then their periods may be irregular or even absent. Females with CF may also have thicker vaginal mucus and this can make it harder for sperm to reach the egg.
Most males with CF have normal sperm production, but the tube that carries them from the testicle to the penis is missing or blocked. Males with CF can have biological children but they will need fertility interventions.
Stress urinary incontinence
Stress urinary incontinence is when urine leaks out during coughing and sneezing. The pelvic floor muscles usually contract automatically with every cough to prevent leakage, but during coughing and sneezing there is increased pressure on the bladder and muscles of the pelvic floor. People with CF are at higher risk of leakage possibly because of the prolonged or chronic cough they experience.
Many people find it embarrassing to talk about stress urinary incontinence. If you are experiencing urine leakage talk to your CF team so they can help you. If the problem remains untreated then it can get worse. Your physiotherapist can advise you about exercises you can do to help with stress urinary incontinence. Controlled coughing and modifications to your airway clearance and exercise routine may be helpful to minimize or prevent leakage.
Bone health
Proper nutrition and exercise are important for healthy bones. All of your bone health and strength is built up during your childhood. Children with CF can have normal bone mineral density when they have a healthy weight, height and good lung function. Physical activity has also been linked to higher bone mineral density levels and improved bone health.
Lung infections in CF can cause inflammation which can contribute to increased bone loss. Poor nutrition leads to lower levels of vitamins D and K, calcium and protein which can cause lower bone mineral density. Certain medications can also cause bone loss to happen more quickly. Your bone mineral density can be measured by a test called a DEXA scan.
Speak to your CF team about how to keep your bones healthy and strong.
Electrolyte imbalance and dehydration
People with CF lose more salt in their sweat which can upset the balance of minerals in their body and lead to dehydration (loss of water), especially with exercise or when the weather is hot. If you are dehydrated you may feel your heart beat faster and you may feel tired or weak. Make sure you drink plenty of water when you exercise and when the weather is hot.
Mental health
Dealing with lifelong illness may cause feelings of fear, sadness and anxiety. Low mood, constant worries or low motivation can block your ability to get things done. Speak to your CF team about what you are feeling. Learn how to support your mental health and well-being.
Clinic appointments
Make sure you attend your CF clinic visit every 3 months. By regularly attending your clinic visits and sharing information you can help your team find solutions early on. If you are not sure, always ask an adult or speak with your CF clinic care provider. If something does not feel right, speak up at the CF clinic, or contact your health-care provider to ask questions.






