Depending on the type and severity of your child's JIA, there are several eye conditions that can affect them including uveitis, cataracts and glaucoma.
Uveitis in JIA
Uveitis is an inflammation inside the eye that can reduce your vision. Uveitis happens with some forms of JIA. It is more common in people with oligoarticular JIA. It does not matter how severe your JIA is. In fact, uveitis is most common in young people with only one or a few joints involved. Uveitis may even start before your JIA is diagnosed.
Uveitis is also not related to how active your JIA is. Your joints can be going through a bad period while your eyes are fine. It is also possible to have severe eye inflammation while the joint inflammation is in remission.
Uveitis can start in one eye and never affect the other eye or it can start in one eye and later involve the other eye. Sometimes, it can start in both eyes at the same time.
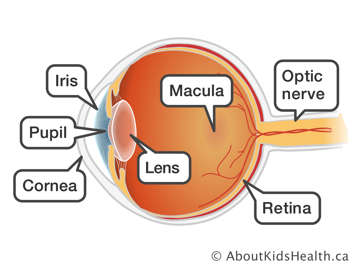
The most common form of uveitis in JIA is known as iridocyclitis or iritis. It affects only the front part of the eye where the colored part around the pupil, called the iris, is located. Iritis often occurs without symptoms and with no visible signs. You may not be aware that you have it. Therefore, it is important to have your eyes checked regularly, even if they are not red or painful. Iritis is treated with corticosteroid eye drops or other medications, including pills, injections, or intravenous medications (depending on the seriousness of the eye inflammation). These treatments protect your eyes and will help prevent blindness.
JIA can sometimes cause uveitis in other parts of your eye. These other types of inflammation are less common but more severe in terms of decreasing your vision.
In the early stages, uveitis may not cause any symptoms, and can only be seen by a special eye exam, which must be done by an ophthalmologist or optometrist. An ophthalmologist is a medical doctor specially trained in eye care and treatment. An optometrist is a health-care professional who can diagnose eye problems. You should have regular eye check-ups by an opthalmologist or optometrist to make sure that your eyes are healthy.
Cataracts in JIA
When the normally clear lens of the eye becomes cloudy, it is called a cataract. Cataracts can affect one or both eyes. Cataracts in young people are rare, but they can occur with JIA. The cloudy lens prevents the rays of light from focusing normally on the retina, which is the lining of the back of your eye. The vision becomes blurry when you have a cataract. Depending on how much and which part of the lens is cloudy, your vision may be mildly or seriously affected.
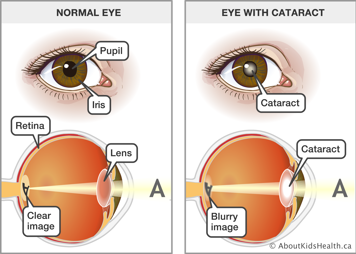
Cataracts can also occur as a side effect of certain medications used to treat JIA, such as corticosteroids (prednisone). These side effects may in part depend on the amount and length of time over which the corticosteroid is used. Some young people seem more sensitive to this than others for reasons we do not really understand. Even though the corticosteroid eye drops used to treat iritis can cause a cataract, the risk of getting a cataract from iritis is higher if these eye drops are not used.
Treatment for cataracts involves surgery to remove the lens of the eye. This is done as a day surgery, meaning that you do not need to stay overnight at the hospital. There are no medications or laser treatments for cataracts and they do not go away by themselves. Some mild cataracts, which do not affect vision, need no treatment at all. For more information on cataract surgery, visit www.pgcfa.org.
Glaucoma in JIA
Glaucoma occurs when the pressure inside the eye is too high. This can damage the optic nerve, which is the nerve that transmits messages from the eye to the brain. Damage of the optic nerve can lead to vision loss or even blindness if not treated. Pressure in the eye can increase either from iritis, or from the corticosteroid drops used to treat iritis.
There are usually no symptoms to warn that you have glaucoma.
Checking for glaucoma should be part of your regular visits to your ophthalmologist or optometrist. Because glaucoma can arise in people with iritis, prevention is key! If you do have glaucoma, you should be under the care of an ophthalmologist. The first line of treatment is eye drops or medication taken by mouth. If that does not work, then you may need surgery. For more information, see www.pgcfa.org.
A story of hope
"I was diagnosed with JIA when I was two and a half years old. My family moved around a lot when I was growing up so I saw a lot of different doctors, all for different problems relating to my JIA. Immediately after being diagnosed with JIA, I was diagnosed with iritis. After being on many eye drops for a long period of time, I developed glaucoma. My rheumatologist was very kind and made sure he did everything he could to help me. Like so many kids with iritis, I sometimes felt lost in the sea of eye drops and noisy waiting rooms. There were some scary moments when my eye's pressure would rise or fall drastically and I would have to go into surgery. Sometimes I would need encouragement to take my eye drops on schedule, or reassurance that my eyes would get better. I always got that support from my family. My eye diseases were very difficult to control at times but with the help from others I have found the strength to face each day with hope."
-Lindsay, young adult






