Acne is a very common skin condition, affecting about 85% of teenagers. Acne is also called “pimples”, “zits” or “blemishes”. You can get acne on your face, neck, shoulders, back and chest.
Teens typically get acne because of hormonal changes that happen along with puberty. Acne usually gets better as you get older, although some people continue to have acne into adulthood.
What causes acne?
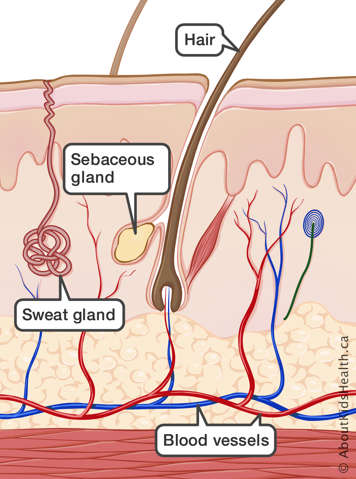
Your skin contains hair follicles (the tunnel that contains a strand of hair) and pores (the opening of the hair follicle on the skin that the hair passes through).
The oil glands in the skin (sebaceous glands) are attached to the side of the hair follicle and release sebum (the oil product of the skin) into the hair follicle to help prevent skin and hair from drying out.
As you go through puberty, hormones can stimulate the sebaceous glands and cause them to make more sebum, which can mix with dead skin cells and clog the pores.
Everyone has bacteria on their skin. A common type of bacteria that lives on the skin is known as Cutibacterium acnes (C. acnes). It sometimes contributes to acne by causing inflammation (redness, swelling and sometimes pus). Having this bacteria on the skin is not a sign of poor hygiene—this bacteria lives on most people’s skin.
Acne can be mild or severe. There are also different types of acne.
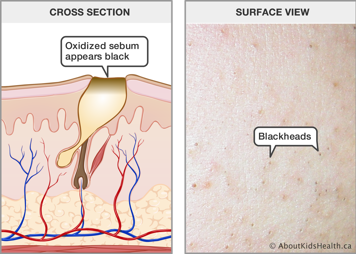
Blackheads (open comedones)
Comedones are pores that are blocked with oil and dead skin cells. A blackhead is also called an open comedone. A blackhead is generally level with the skin surface but cannot be removed by normal face washing. They appear black because the oil oxidizes when it comes into contact with open air.
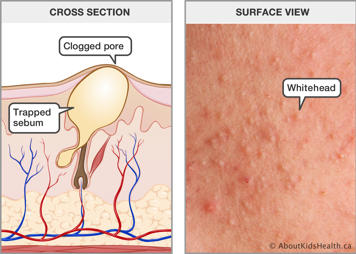
Whiteheads (closed comedones)
A whitehead is another type of comedo. It’s slightly raised from the skin but there’s no redness or inflammation. It may look like there is a core of white material or the bump might look like the same colour as your skin.
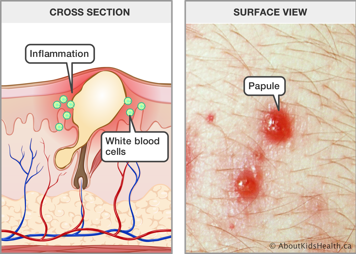
Papules
Papules are red, small, hard bumps that are slightly raised on the skin. Papules happen because white blood cells enter the follicle, causing inflammation. White blood cells help to fight infection.
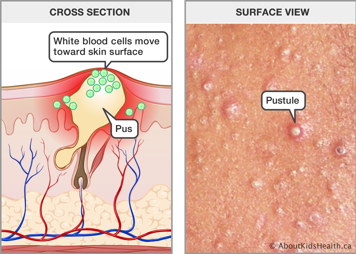
Pustules
When the white blood cells in a papule make it to the surface of the skin, a pustule is formed. Pustules look like red, inflamed circles with a central, raised bump that is yellowish or white. The bump is filled with pus. Pus is caused by inflammation. It contains white blood cells, dead skin cells and bacteria.
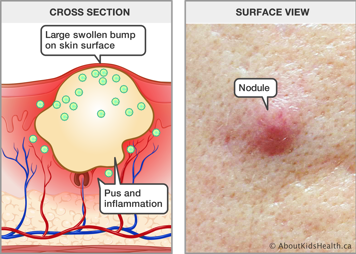
Nodules
When a papule or pustule gets bigger, it can cause more severe inflammation in the surrounding skin. This can lead to nodules, which are deep, red, round bumps that can be as big as 6 to 20 millimetres. They are sometimes called cysts.
Nodules are formed by irritated, inflamed hair follicles that have ruptured, or broken, deep under the skin. They can be throbbing and painful, even without touching.
How can I treat acne?
Treatment depends on the severity and type of acne. An effective treatment will help reduce future breakouts and improve the skin's appearance. Keep in mind that it may take up to four to six weeks of treatment before you start to notice a result. The full benefit of a treatment might take four to six months of treatment. Severe acne may need longer. You may need to try several different treatments to find the one that is right for you.
In most cases, your health-care provider or dermatologist (a doctor who treats skin conditions) will prescribe topical treatments (medicines in cream, gel or lotion applied directly on the skin). For more severe acne, they may prescribe an oral treatment (taken by mouth).
Cleansing skin
Acne is a process deep within the skin. Washing your face regularly helps remove dead skin cells and excess oil but doesn't play a significant role in preventing or managing acne.
Sometimes, medicated cleansers are used as part of acne treatment. These products can often be purchased without a prescription but can be irritating or may not be the right choice for your acne. Your health-care provider can explain if these cleansers are a good choice for you.
If you have acne, avoid scrubbing your face when washing because this may make inflammation and irritation worse. Instead, gently wash your face with warm water. You may also use a mild cleansing product if you want.
Topical medications
Topical retinoids
Topical retinoids unplug comedones and improve the process of shedding the old skin cells. They may also help reduce any inflammation. They can also reduce the number of new acne lesions that develop. Retinoids can cause deep but hard-to-see comedones to come to the surface and look more inflamed and noticeable. This is often called "purging". It is the way that retinoids work and most commonly occurs in the first few weeks of using the medication. Sometimes that makes it seem like the medication is making acne worse, but it is actually part of the treatment and usually settles down within a few weeks.
Some side effects may occur when using a topical retinoid. These include:
- mild irritation
- redness
- dryness
- peeling
- sensitivity to sun
If you are pregnant, or thinking about having a baby, talk to your health-care provider before using a topical retinoid as they should not be used during pregnancy.
Use regular sun protection on exposed skin treated with retinoids.
Avoid skin damage, such as waxing, laser or exfoliation (e.g., facials, scrubs), in the areas where you are applying retinoids.
Retinoids are available in many strengths and formulations. There is no one “better” option; your health-care provider will recommend a retinoid that is most appropriate for you.
Topical anti-inflammatory medications
Topical anti-inflammatory medications are used to reduce inflammation and can reduce bacteria that contribute to inflammation. One option is benzoyl peroxide, which is available over the counter.
Use caution when applying benzoyl peroxide because it is a strong bleaching agent that can damage fabrics. In rare cases, it can cause an allergic reaction, which could cause significant redness, swelling and/or itching.
Topical androgen blockers
Clascoterone helps block androgens (hormones) from causing the sebaceous glands to secrete excess sebum (oil). The medication can also help reduce inflammation. Unlike many of the other topical medications, this one is used two times per day.
Oral medications (medications by mouth)
Oral antibiotics
An oral antibiotic is sometimes used for treating more significant acne, which is mostly made up of inflammatory papules or nodules. Just like topical treatments, oral antibiotics reduce inflammation. Taking antibiotics for a long time can cause problems; for example, it can disrupt the normal bacteria of the gut or cause some bacteria to become resistant to the antibiotic. To reduce these risks, most health-care providers will recommend only using these medications for a short time.
Hormonal therapy
Treating acne with an oral contraceptive (birth control pill) is an effective treatment option for some female patients. This type of treatment limits sebum secretion by reducing androgen levels. Other topical and oral treatments can be used along with oral hormonal therapy.
Treating acne using hormones is not for everybody. For more information, talk to your health-care provider.
Oral isotretinoin
Isotretinoin (known as Accutane® in North America; Clarus®, Epuris®, Absorbica® in Canada; and Roaccutane® in Europe) is a chemical compound related to vitamin A. In most cases, isotretinoin is used to treat severe nodular and scarring acne because it:
- reduces sebum secretion
- prevents comedones from forming
- acts as an anti-inflammatory
- stops C. acnes from multiplying in hair follicles and sebaceous glands
However, this type of acne treatment must be closely monitored because isotretinoin has several side effects. More common side effects include dry skin, lips, nose and eyes. All side effects will start to disappear when treatment stops.
However, there are more severe side effects. For example, isotretinoin can interfere with the development of a fetus. If you are pregnant or thinking about having a baby, talk to your health-care provider about the side effects of isotretinoin. There are also concerns about depression, headaches, joint or muscle aches and pains, and impact on the liver.
Combined treatment
A combined treatment can be an effective way to treat acne. A topical retinoid and an anti-inflammatory cream or gel can be used together. Sometimes, they are combined in one product. Other times, they are used as two different products. For example, a topical anti-inflammatory may be applied in the morning and a topical retinoid may be used at night.
Oral medications are also used in combination with a topical treatment. Many people taking a pill will get added benefit from also using topical medication.
Your health-care provider will advise you on how and when to use a combined treatment for acne.
Scar prevention
Handle acne with care. Manipulating, squeezing and popping increases the likelihood of scarring. The best way to prevent scarring is to actively treat the acne and avoid manipulating the lesions.
When should I talk to a health-care provider?
If you have any questions about how to treat your acne or if it’s causing you stress and worry, talk to your health-care provider. They may be able to help you, or they can refer you to a dermatologist.
Treatment is not only for those who have severe acne. No matter how little or how much acne you might have, you can seek treatment for your skin.
