The management of hemophilia has changed significantly since doctors started using a type of replacement therapy in the 1950's.
1950s and early 1960s
Doctors treated bleeds in patients with hemophilia by replacing the missing factor with clotting factor found in whole blood and fresh frozen plasma. This proved that some type of “replacement” therapy could work.
However, these treatments came in large volumes that contained very little factor. Also, products needed to be kept in the hospital in a freezer.
1958
For the first time, doctors treated hemophilia using prophylaxis. A Swedish doctor, Dr. Inga Marie Nilsson, gave a patient blood product on a regular basis to prevent bleeding.
1960s
Scientists and doctors started to better understand bleeding and clotting. This helped them identify and name blood proteins, called factors.
They also started treating people with hemophilia with higher concentrates of factor, which they collected by taking fresh frozen plasma and thawing it at a low temperature. This form of factor was called cryoprecipitate. Patients with hemophilia A took cryoprecipitate that contained factor 8 (VIII); now they could get enough factor to stop the bleeding.
1968
Doctors treated people with hemophilia with even higher concentrations of factor by drying it at very low temperatures (freeze-drying). These preparations of factor are called blood-derived factor concentrates.
Patients stored these factor concentrates in the fridge so they did not have to go to the hospital for product anymore. However, freeze-dried factor was still made from blood plasma, which meant that the factor might be contaminated with viruses.
1969
Canada’s first comprehensive care team (CCT) began taking patients in Montreal.
Early 1970s
It was common for people living with hemophilia to take prophylaxis as treatment.
1977
Doctors treated mild hemophilia A using a man-made hormone called desmopressin (DDAVP). DDAVP triggers the body to release two factors on its own: factor 8 (VIII) and von Willebrand factor. It was inexpensive. But doctors still did not have treatment for hemophilia B.
Mid and late 1980s
Patients used safer factor concentrates. New manufacturing practices inactivated viruses such as HIV and hepatitis C that contaminated factor concentrates. However, factor was still derived from blood plasma so it could transmit other types of infections. Donor screening was also introduced.
Early 1990s
Researchers made clotting factors inside the laboratory, and no longer needed to extract factor from human plasma. Factor produced in the lab is called recombinant factor.
1993
Doctors started using recombinant factor 8 (VIII) to treat hemophilia A.
1997
Doctors could treat hemophilia B with recombinant factor 9 (IX).
2002
One of the most celebrated hockey icons in Canadian history, Mario Lemieux, becomes the Honorary President of the Canadian Hemophilia Society (CHS).
2006
In Canada, 69% of people living with severe hemophilia A use prophylaxis.
2014
Longer-acting factors become available.
2016
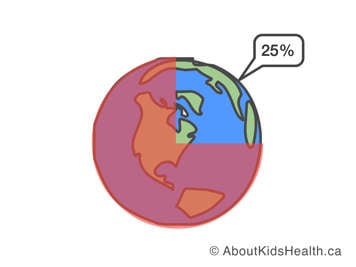
Currently, only about 25% of people with hemophilia in the world have access to treatment.
Accessing hemophilia care
Part of managing hemophilia is being able to access a wide range of health-care professionals that address all aspects of the disease; this is called comprehensive care. These health-care professionals include your hemophilia specialist physician, nurse, physiotherapist, social worker and others. In addition to the team in your hemophilia treatment centre, you will also need to be able to interact with emergency room personnel for acute issues and your family doctor for routine non-hemophilia health care.
Approximately 400,000 people from every ethnic background across the world are affected by hemophilia. For years, only 80,000 of them people living with hemophilia (20%) received comprehensive care. But with continued improvements in access to care, close to 25% of people living with hemophilia now receive comprehensive care. This still leaves about 300,000 people living with hemophilia around the world with little or no care.
The main reason for this is the high cost of treatment. Despite the hassles of living with a bleeding disorder, consider the benefits of your treatment and how it improves your life. In the future, we hope all people with hemophilia will have access to comprehensive care.
